Lisa Summers,Scotland health correspondent and
Andrew Picken
 Lori Quate
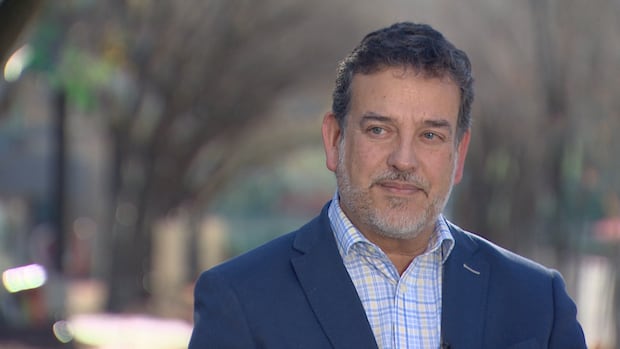
Lori QuateJust a week before she was due to give birth, Jacqui Hunter was given the devastating news that her daughter had died in the womb.
Less than 24 hours later, Jacqui was also dead.
The 39-year-old had been told she would have to give birth to her stillborn daughter, who was called Olivia, and was given medication to bring on the labour.
Within hours Jacqui was having intense contractions and at one point slumped into the arms of her husband, Lori Quate, who thought she had fainted.
As staff at Ninewells Hospital rushed to help her, she suffered a cardiac arrest.
Jacqui died two hours later from an amniotic fluid embolism – a rare and life-threatening emergency.
It was not until the next day that Lori found out his wife had been given eight times the recommended dose of the drug to bring on labour – a mistake which some experts say may have contributed to her death.
Lori is one of dozens of people – families, midwives and experts – who have told a BBC Disclosure investigation that urgent action is needed to improve maternity safety in Scotland.
They shared details of many of examples of poor and sometimes deadly care, with NHS resources increasingly stretched.
The Scottish government say “significant progress” has been made in the last 20 years in reducing infant mortality and neonatal deaths, while a new programme of maternity unit inspections is helping to raise standards.
But there are calls for a national review similar to one being carried out in England, where a series of independent reviews have found that hundreds of mothers and babies could have survived with better care.
 Fern Photography
Fern PhotographyThe devastation of losing his wife and baby in the space of 24 hours is still firmly etched on Lori’s face five years on from the tragic incident.
He says his wife was let down “in the most horrific way”.
Jacqui was not told she had been given an overdose of Misoprostol, the drug used to bring on labour, even though some staff were aware of the error before her contractions started.
Lori says that in Jacqui’s medical notes there is no mention of the drug error until after she was declared dead.
He says, “Not going to Jacqui, their patient, and saying we have messed up. Jacqui had a right to know about that, and they kept it from her.”
 Lori – Mark Quate
Lori – Mark QuateAn investigation into Jacqui’s death in 2020 was carried out by an NHS Tayside review panel. It acknowledged that amniotic fluid embolism (AFE) “can occur in any labour and it is not possible to be certain that in this case an AFE would not have occurred with the correct dose of Misoprostol”.
But the panel added that “as it is known that higher doses of Misoprostol increase the risk of AFE, the incorrect dose must be considered as a major contributing factor to AFE and subsequent death”.
The panel also said Jacqui should have been informed of the medication error.
A fatal accident inquiry was then carried out, which published its findings last year. It concluded that it was possible, but not probable, that Jacqui’s death could have been prevented if she had been given the correct dose.
The inquiry also made no finding in respect of discussing the overdose with Jacqui.
A spokeswoman for NHS Tayside said it was “deeply sorry” for Lori’s loss and had carried out a number of internal investigations, and taken part in external reviews, following the death.
“All recommendations identified in the reviews were fully accepted and, as a result, our systems and processes have been strengthened where required and improvements have been made to how we provide care,” she added.
Lori fears that failings in maternity care in Scotland are not being examined in the same way that services are reviewed in England.
He wants a Scotland-wide review similar to the one which is examining 2,297 cases of harm to babies and women under the care of Nottingham University Hospitals NHS Trust.
Baby and maternal deaths are rare in Scotland but while making this documentary, we heard time and again from families, experts and staff about the challenges being faced by maternity and newborn baby services.
We spoke to families left angry because they had to fight for answers after going through devastating experiences.
They also feel shut out by health boards who they believe are more concerned with reputational damage than honesty and transparency.
Staff members tell us they are working in conditions that are often not as safe as they should be for women and babies – sometimes due to understaffing, sometimes because less experienced employees have had to take on additional duties.
Like the rest of the UK, Scotland has seen an increase in Caesarean sections, inductions of labour, serious tears during childbirth and the proportion of babies born in poorer health.
There have also been several spikes in neonatal deaths in recent years.
These are clues that the system is not working as well as it should.
Experts say there is no reason to believe Scotland is any different to other parts of the UK, where a series of independent reviews have identified common failings relating to staffing, poor workplace culture, listening to families and learning from mistakes.
There are two independent safety investigation and inspection bodies in England, which are regularly reporting on their findings.
In Scotland, the last major review of maternity care was in 2017 after a BBC investigation revealed a number of babies had died at Crosshouse Hospital in Kilmarnock.
In 2022, a targeted investigation was launched into two spikes in the neonatal death rate over a six-month period.
It found no evidence of systematic failures in care but noted that some deaths may have been preventable.

The report’s publication in 2024 led to the introduction of independent inspections of maternity units for the first time.
The first review was at Ninewells Hospital, where Jacqui and Olivia died. It found a series of patient safety concerns, including staffing shortages and delays in assessing expectant mums.
If a serious incident which affects patient safety takes place in any hospital or healthcare facility, the health board can decide to carry out a Significant Adverse Event Review (SAER).
These internal investigations are used to learn from incidents and try to prevent them happening again.
There have been 143 SAER reviews related to maternity care in total since 2020 with the most, 44, occurring in NHS Greater Glasgow and Clyde.
By contrast, England’s Maternity and Newborn Safety Investigations programme completed 613 independent safety investigations in 2024/25 alone.
 Julie Keegan
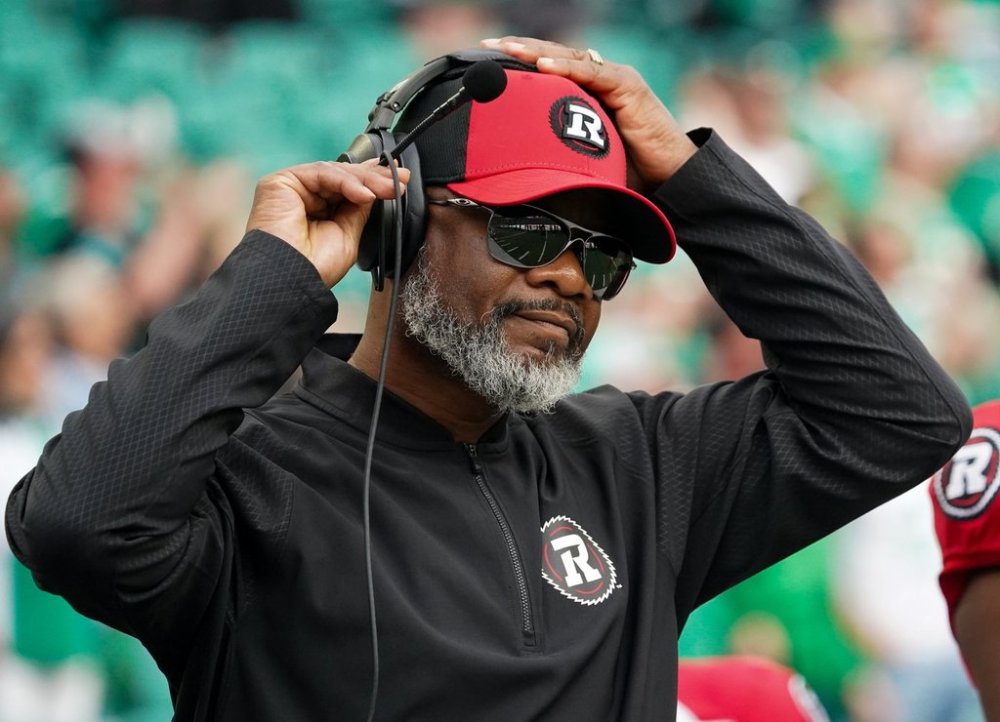
Julie KeeganOne of the maternity SAER reviews carried out was after the death of three-day-old baby Mason Scott McLean in 2023.
His parents Julie and Angus had been elated after his birth in Glasgow’s Princess Royal Maternity Hospital.
But shortly after being sent home the next day, they noticed Mason was lethargic and no longer interested in feeding.
A community midwife visited and, after carrying out routine checks, offered reassurances but the couple remained concerned so they took Mason to the emergency department at the Royal Children’s Hospital that night to be checked.
Julie is an NHS intensive care nurse and used to looking after patients who need critical care.
But she felt nobody grasped how serious things were for Mason: “It was the most basic nursing care and they would have known how sick he was.”
 Julie Keegan
Julie KeeganAfter three hours in accident and emergency, Mason was transferred to the neonatal unit – but critical information wasn’t passed on.
Julie remembers hearing a gasp from Mason.
“I think it was his last breath. Angus asked the doctor… is he still breathing?”
Julie says that when the doctor could not get bloods, she realised Mason wasn’t breathing – and says the medic then “went into total panic”.
Baby Mason’s death was caused by sepsis and related feeding issues after being in the hospital for six hours.
NHS Greater Glasgow and Clyde produced a SAER into his death.
It concluded that staff recorded Mason’s temperature incorrectly and his records were incomplete, meaning staff failed to recognise how sick he was.
Mason had hypothermia but equipment wasn’t sourced to heat him up.
And key tests were missed that would have indicated he had a life-threatening infection.
The SAER review pointed to “several systematic issues” that may have caused Mason’s death.
“You just think, are the mistakes going to happen again?” Julie adds.
NHS Greater Glasgow and Clyde said it had “undertaken to action the recommendations identified in the SAER” including updating its neonatal guidance.
A spokeswoman extended the health board’s “heartfelt condolences” to Mason’s family.
“The report recognises, despite staff documenting concerns raised about Mason, that there were some missed opportunities for care, and we are very sorry for this,” she said.
The health board also said it was introducing new infant feeding guidance, which was now going through the appropriate approval process.
Retired consultant neonatologist Dr Helen Mactier was the author of the review of neonatal deaths in Scotland which was published last year.
She says families affected by poor maternity care are looking for an apology and an “open and an honest” account of what happened.
Dr Mactier believes that improvements are still needed in the way the deaths of newborn babies are investigated – and that some issues are common across the whole of the UK.
“We find that serious adverse event reviews are not always undertaken quite as thoroughly as they might be and that the learning from these reviews is not always made,” she says.
“It’s very concerning that review after review says essentially the same thing. It says that we commonly fail to listen to patients.”
“We get so tied up in protocols and systems and processes, that we actually forget to use our ears and listen to what the patient’s telling us.”
Dr Mactier says action, rather than more reviews, is what is needed to tackle “the systemic issues” and improve care for patients.
Public Health and Women’s Health Minister Jenni Minto said Scotland had made “significant progress” in reducing infant mortality, neonatal deaths and stillbirths in the last 20 years.
She said: “We are committed to learning from every case to improve care, strengthen safety, and support women and their families.
“We are providing record funding to NHS boards and have strengthened guidance on SAERs to ensure lessons are learned and care improves continuously.”
She also welcomed Healthcare Improvement Scotland’s decision to conduct unannounced inspections of all obstetric units.
“In addition, we have commissioned HIS to develop a set of national standards for maternity care, which are expected to publish shortly,” she added.
Minto pointed to safe staffing legislation and all pregnant women being allocated a primary midwife as examples of initiatives which were raising standards of care.
If you have been affected by the issues raised in this story, information and support can be found at the BBC’s Action Line.